Essential thrombocythemia (ET) is one of the myeloproliferative neoplasms with a high risk of progression to post-ET myelofibrosis (post-ET MF). However, there still lacked the prediction model of post-ET MF. Here, we conducted a study of 708 ET patients identified by 2016 WHO diagnostic criteria in 13 hematology centers between 01 January 2010 to 01 July 2023, aimed to identify risk factors progression to MF and develop a prediction nomogram for post-ET MF(ChiCTR2200061208).
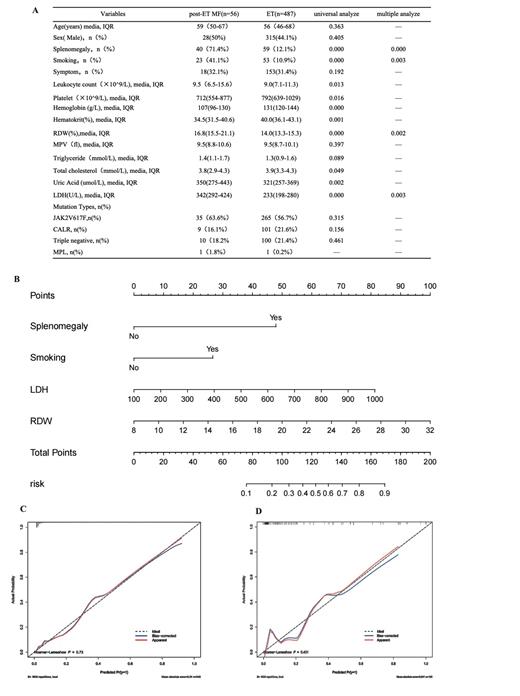
The training cohort included 543 ET patients with ET from 8 hematology centers. The external validation cohort included 165 subjects from another 5 hematology centers. Univariable and multivariable analysis identified the red blood cell distribution width (RDW) level (P=0.002), lactic dehydrogenase (LDH) level (P=0.003), smoking(P=0.003) and splenomegaly (P=0.000) were independent risk factors of post-ET MF(Table A). These independent risk factors were included to develop a prediction model of nomogram (Figure B). The bias-corrected AUC were both high in the training cohort (AUC=0.899) and external validation cohort (AUC=0.892). Analysis of calibration curves showed that the apparent and bias-corrected lines were overlapped with the ideal line in both training and external validation cohorts, and the Hosmer−Leeshawn tests showed that the model were a good fit (P = 0.73 in training cohort, P=0.43 in external validation cohort) (Figure C, D). Decision curve analysis(DCA) was conducted to assess the clinical usefulness of nomogram by quantifying the net benefits at defferent threshold probability of post-ET MF. Threshold probabilities for the standardized net benefit nomogram in predicting the probability of the occurrence of post-ET MF ranged from 0.02 to 0.87 in the training cohort, 0.01 to 1 in the external validation cohort.
In conclusion, we developed a nomogram that can predict the risk of progression to MF in ET patients, which can help clinicians adjust therapy timely to prevent disease progression to a great degree.
Acknowledgement: This research was funded by the Key R&D Program of Zhejiang, No. 2022C03137; Public Technology Application Research Program of Zhejiang, China, No. LGF21H080003; Zhejiang Medical Association Clinical Medical Research special fund project, No. 2022ZYC-D09.
Correspondence to: Dr Jian Huang, Department of Hematology, The First Affiliated Hospital of Zhejiang University School of Medicine. No. 79 Qingchun Road. Hangzhou, Zhejiang, PR China.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal